I am 10 weeks post abdominoplasty and recovery has been challenging, just not in the ways I originally anticipated. Going into surgery, I was concerned about things such as implications to my pelvic health function (no history of symptoms, but was concerned about the potential of them due to pressure changes), and long term athleticism. These are absolutely still considerations, but these were the variables I was prepared to “counter” with education, strategy, and support from the professionals in my life.
Overall, I am doing very well. I have not experienced pain with this procedure... discomfort? Yes, initially, and sporadically, but nothing lingering or too consuming. For more context, you can read about my first week recovering, and about coming to this decision to begin with, here.
I had a very difficult time finding a compression garment that did not irritate my incision post op. It seemed like no matter what I wore, it rubbed and created a lot of irritation during a critical healing process. The problem was I wanted to make sure that the internal stitches down my linea alba were supported during the healing process with all the swelling, so I NEEDED to wear compression as most surgeons recommend. However, because of how low my scar is, the bottom of the compression garments sat on top or right over, rubbing with any movement. That seemed to be the beginning of the challenges with the healing.
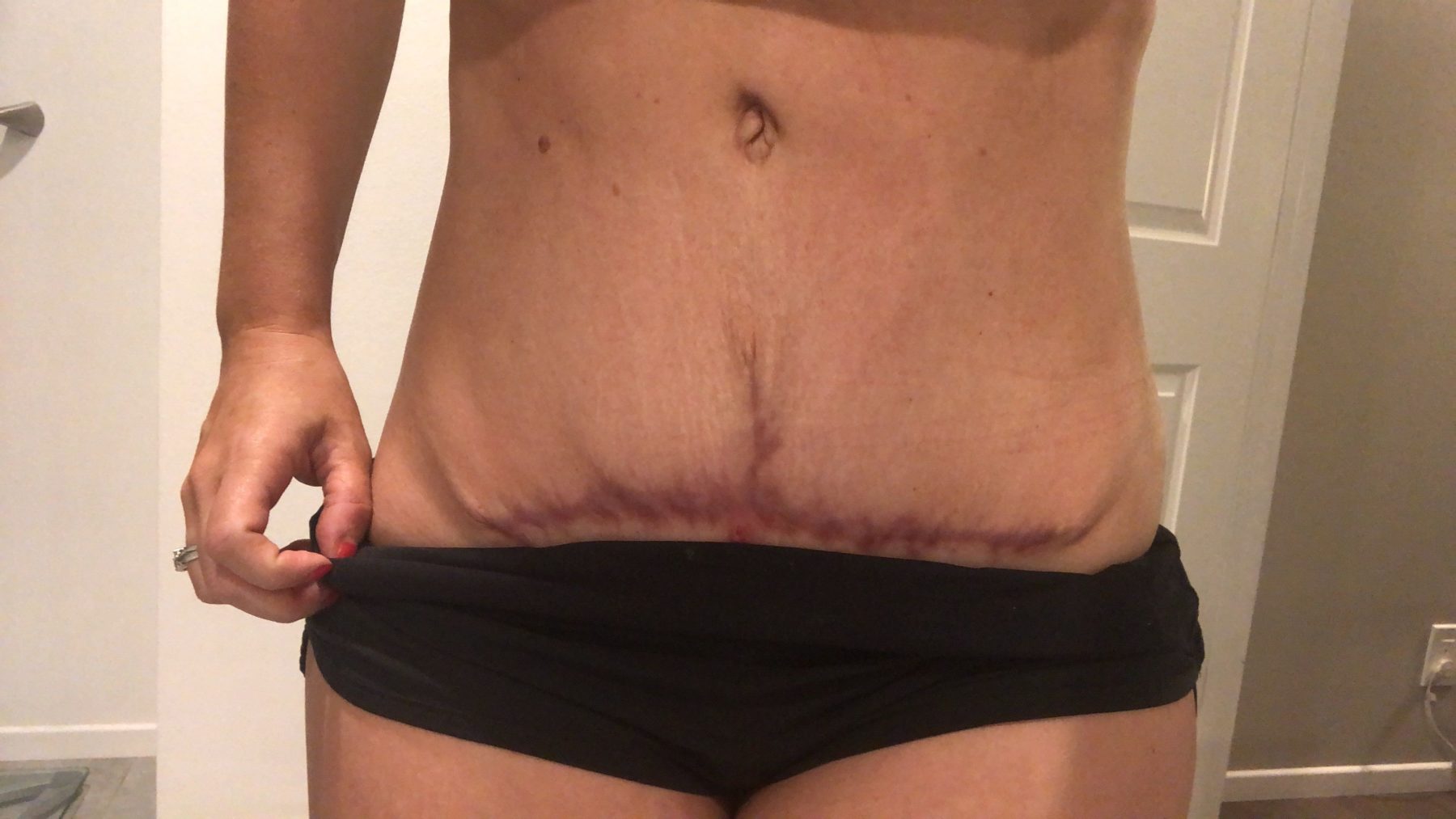
I’ve had a hard time healing externally, between the rubbing of the garments, the low location of my particular scar (we used my C section scar which was very low), and the fact that I did not have a lot of loose skin/fat to pull down created a lot of tension on this scar and healing process. Tension + swelling + irritation had led to some dissolvable stitches “popping” or more like, being exposed, which led me to getting them removed by a registered nurse. This was around 6 weeks post op and since then, my scar has “spread” instead of being a thin line. It is redder and wider from it becoming opened, scabbing, etc. This is referred to as a “delayed healing” and impacts the long term appearance of scars. We (Dr. Jamie and I), also hypothesize that perhaps I had a reaction to sutures and this affected the healing process. Either way, there were quite a few variables and wound management is such a hard thing to troubleshoot (we tried many things) and were in constant communication.

This is frustrating. It’s not just about appearance because I know with TIME, it will improve in color, but it’s the trauma it experienced, the thickness/wideness of it and the maturation of how scarring works that’s concerning for this significant of a scar and the area it’s in. I want my scar to heal well, and it has gotten off to a less than ideal start.
I value my body, it’s function, the process and the long term effects of what I do to my body. I understand that there are variables that can’t always be controlled and so far I’m grateful that the “big picture” variables of function are progressing well.
When I go back to Tuscon, AZ to see Jamie for my 3 month follow up, I will also be getting a scar revision to give my scar the best possible long term healing chance. Addressing it sooner (under MY particular circumstances) is recommended. Yes, I could wait, but ultimately, this scar needs a revision (excision of the current scar, and new sutures, using a different material to be safe). This is a superficial procedure, so much less invasive than the original abdominoplasty where I was totally opened up. This will address the wideness/spreading that it has experienced, the “dog ears” on the ends (which needed revision eventually anyway) and the overall appearance without the variables of being sutured under max tension + swelling + need for compression.
If you’re like, “But Bri, is this really what the best option is? Can’t you give it more time?” Oh trust me, I’ve been working through this question myself for a while now. So I have done what I always do when I’m uncertain... I ask a LOT of people a LOT of questions.
I have sought out two other plastic surgeons opinions, multiple pelvic floor physical therapists and medical pros... and they all agree that a revision is ideal, and to do it earlier in THIS particular circumstance (we know what caused the variables of trauma, we can control those variables this time and give the scar a better chance to heal earlier rather than going through the healing process and then starting it over again). I was told that color would improve over time, but wideness and how it spread would not improve, even with laser.
This is hard to explain, frustrating, but it seems like there’s always variables that impact how women heal from this procedure. There are so many things I don’t know, and I try to be transparent in this because I know there's a certain amount of professional responsibility I carry to “do the right thing.” I’m trying but I’m also working through a process that’s new and unfamiliar. I’m in the trenches and I’m not ready to offer an “expert opinion” on ANYTHING... yet. I may have a good understanding of the system and athletic progression (that part is going well!), but the surrounding variables are kicking my ass mentally and emotionally.
Speaking of training, I began exercising around 8 weeks post op (after those sutures had been removed and the scar had formed a scab in those opened areas).
Before then, I had gone to pelvic floor physical therapy and progressed my activities of daily living in a way that mirrored rehab and fitness demands. For example, picking up Chance a couple of times a day, then eventually holding him for a while longer, then walking carrying him, etc. That’s just ONE example, but it was also making sure I could connect my breath/TA/PF to movement demands (getting out of bed, getting the stroller out of my car, lifting kids/things off the floor, etc). Progressive overload is applied to LIFE.
At 10 weeks my training is about moving, not jumping back in, not ab work or high intensity. It’s sweating, getting familiar with my body and not stressing it beyond readiness. If I second guess something, I don’t do it. I’ve become good with my athlete brain, but it isn’t a perfect process.
It will be frustrating to step back from training again when I’m recovering from the revision, but I trust that my now is on behalf of my later and that I am strong enough mentally and physically to step back.
Thank you for reading and for your support. This feels embarrassing, overwhelming and like a lot of responsibility to share publicly, but I also know these variables were a bit out of my control. I’m moving forward with the knowledge and circumstances in the ways that I do have control over... choices, information and long term outcome, not short term desperation.

Thank you for sharing all this with us, step by step, and not flossing over or leaving out completely the pain, frustration, concerns and your decision process. You don’t owe it to us ( or anyone) but it is greatly appreciated. I am currently pregnant with baby #4 (totally unplanned) and I found you while pregnant with my 3rd and I am so grateful for you and all your information. I workout regularly and lift heavy and am incredibly competitive. I KNOW FOR A FACT that I would have overdone it and probably done some damage to my PF or abdominals had you not equipped me with proper knowledge about pre and postnatal fitness. Also you gave me the freedom to say “No, I’m not doing that. That’s not safe.” As well as a constant reassuring voice telling, “go slow. There’s time. Respect the process. Don’t rush. Slow is smooth and smooth is fast”. I knew what to do then with my 3rd and I am confident about what to do with this pregnancy. You’ve also helped to accept that if I am careful and wise about my body, how to use it, how to strengthen it, how to care about and for it, then how it looks in the end is EXACTLY how it’s supposed to look. Thank you and I pray you have a safe and successful scar treatment and recovery.
I’m super curious about connecting breathing/pf/ta to work loads post surgery. My surgery is less than two months away and aside from recovery concerns, I’m also aware and concerned about pf changes. I’ve come a long way and hope I don’t go backwards. Was it something you had to self-talk and think about before adding the work loads? Do you have any strategies when you are first starting?
Thanks!
I also made the decision to have this same surgery. It was the best decision I’ve ever made. Although I didnt necessarily think so for about the first year. Now 4 years later I am the strongest I’ve ever been in my life and I never even think about it.